Wisdom Teeth FAQ

What are wisdom teeth?
Wisdom teeth – also known as third molars – are the teeth in the very back of your mouth behind your other molars (1st molars and 2nd molars). They typically appear in the mouth for the first time between the ages of 17 and 25, but they are not required for adequate chewing function.
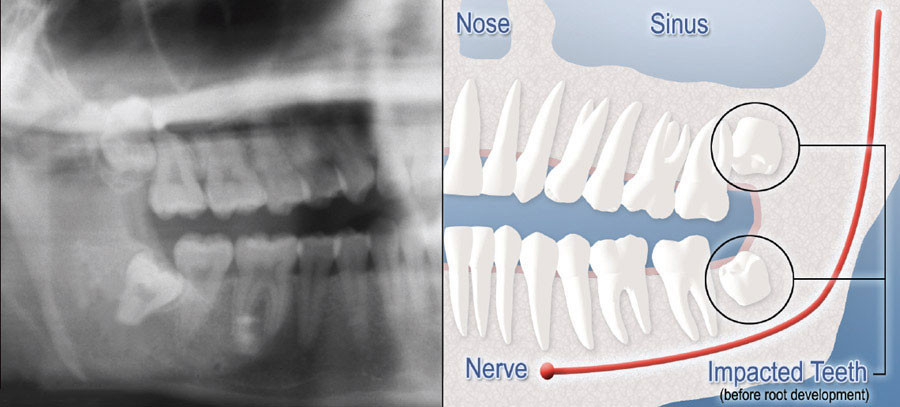
What is an impacted tooth?
Although most people develop and grow 32 permanent adult teeth, many times their jaws are too small to accommodate them all. When inadequate space prevents the teeth from erupting they are called impacted wisdom teeth. This indicates their inability to erupt into the proper position for chewing and cleaning. Since wisdom teeth are the last ones to come into the mouth, they’re the most likely to become impacted when there’s not enough space, however this can happen to other teeth as well.
Why do we have wisdom teeth?
 This is a great question. There is no clear answer, but there are several prominent theories. One theory is that we evolved from a species with larger jaws than we now need, but the number of teeth we make has not kept up with that evolution. Another theory is that before modern dental care and water fluoridation, people were more likely to lose their first molars to decay (cavities) – allowing the second and third molars to shift forward into a functional position. A further theory is that the food we eat has become softer and easier to chew, resulting in less grinding/wear of our molars.
This is a great question. There is no clear answer, but there are several prominent theories. One theory is that we evolved from a species with larger jaws than we now need, but the number of teeth we make has not kept up with that evolution. Another theory is that before modern dental care and water fluoridation, people were more likely to lose their first molars to decay (cavities) – allowing the second and third molars to shift forward into a functional position. A further theory is that the food we eat has become softer and easier to chew, resulting in less grinding/wear of our molars.
Does everyone have wisdom teeth?
No, in fact, some people never grow any wisdom teeth! Somewhere between 5.5% and 37% of the population is missing at least one wisdom tooth.
Why should I have my wisdom teeth removed?
If you do not have enough room in your mouth for your third molars to fully erupt, a number of problems can occur with them. Impacted wisdom teeth should be removed before their root structure is fully developed. In some patients it is as early as 12 or 13, and in others it may not be until the early twenties. Problems tend to occur with increasing frequency after the age of 30. Some of the possible problems related to not removing your wisdom teeth include:
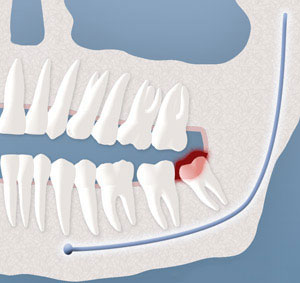
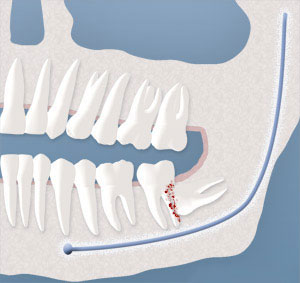
Infection:
The most frequent clinical problem we see is pericoronitis, (a localized gum infection). Without enough room for total eruption, the gum tissue around the wisdom tooth can become irritated and infected, resulting in recurrent pain, swelling, and problems with chewing and/or swallowing.
Cyst Formation:
Non-infectious diseases may also arise in association with an impacted wisdom tooth. Cysts are fluid-filled “balloons” inside the jaw bone that develop as a result of impacted teeth and slowly expand destroying adjacent jaw bone and occasionally teeth. They can be very difficult to treat if your wisdom teeth are not removed in your teenage years. Although rare, tumors can be associated with the delayed removal of wisdom teeth.
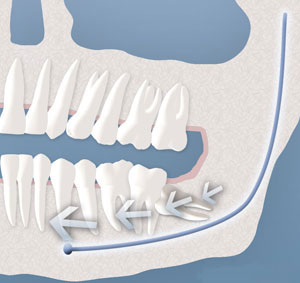
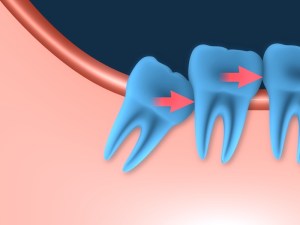
Possible Crowding:
Impacted wisdom teeth may contribute to crowding of your teeth. This is most noticeable with the front teeth, primarily the lower front teeth and is most commonly seen after a patient has had braces. There are a number of factors that cause teeth to crowd after braces or in early adulthood. Retained, impacted wisdom teeth may be a contributing factor. Unless you have an active problem when you see the oral surgeon, the reason for removal is primarily to prevent long-term damage to your teeth, gums and jaw bone.
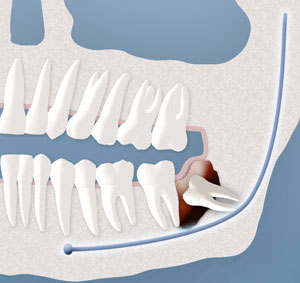
Damage to Adjacent Teeth:
If there is inadequate room to clean around the wisdom tooth, the tooth directly in front, the second molar, can be adversely affected resulting in gum disease, bone loss around the tooth, and/or decay.
Does everyone need to have their wisdom teeth removed?
No, not everyone needs to have their wisdom teeth removed. If you have enough space for them to erupt normally and clean and maintain them, then removal is not required, however this only applies to about 15-35% of the general population. There are many reasons your dentist may have recommended this treatment. For example, cavities (decay), gum disease (periodontal disease), cysts of the jaws, compromise of adjacent teeth (2nd molar), orthodontic crowding, or they are impacted and it is judged that you will not have sufficient space in your mouth for them to erupt normally. To determine if you should have your wisdom teeth removed, Dr. Robertson will evaluate them clinically and assess them on a panoramic radiograph, which shows the whole mouth.
Can my regular dentist take out my wisdom teeth?
Some general dentists can remove straight forward wisdom teeth, but the more complex or impacted teeth are best managed by a specialist oral surgeon. Specialist oral surgeons regularly handle wisdom teeth removal and are fully equipped to perform complex surgeries with minimal risks. There is a higher risk of complications with an inexperienced provider (such as nerve injury, see below), so having your wisdom teeth removed by a surgeon who does the procedure many times every day is usually your safest bet. Dr. Robertson removes thousands of wisdom teeth every year.
What is the best age to have my wisdom teeth removed?
 Once the wisdom teeth start to cause pain or other symptoms, they should be evaluated right away. However if they haven’t caused pain yet, they may still be recommended for removal for preventative reasons at the ideal stage of development (when the wisdom teeth have one half of their full root development). The age associated with that stage of development is different for everyone, but generally occurs between 15 – 22 years old. The best way to determine the ideal time for your procedure is forDr. Robertson to review your recent panoramic radiograph. If you or your dentist are unsure about the best age, send a recent panoramic radiograph to us and Dr. Robertson will give you an opinion, free of charge, over email, so you can decide if you’d like to come for a consultation.
Once the wisdom teeth start to cause pain or other symptoms, they should be evaluated right away. However if they haven’t caused pain yet, they may still be recommended for removal for preventative reasons at the ideal stage of development (when the wisdom teeth have one half of their full root development). The age associated with that stage of development is different for everyone, but generally occurs between 15 – 22 years old. The best way to determine the ideal time for your procedure is forDr. Robertson to review your recent panoramic radiograph. If you or your dentist are unsure about the best age, send a recent panoramic radiograph to us and Dr. Robertson will give you an opinion, free of charge, over email, so you can decide if you’d like to come for a consultation.
Should I be put to sleep to have my wisdom teeth removed?
You can elect to have your wisdom teeth removed with freezing (local anesthesia) or IV sedation, but generally patients prefer to be put fully to sleep (general anesthesia) for this type of procedure. With general anesthesia, you’ll wake up in the recovery room after the procedure is finished and you can simply focus on healing. The procedure can be done faster and more precisely whilst you are asleep, so you will have less swelling after surgery (swelling is directly related to surgical time) and you’ll recover faster.
Is general anesthesia safe?
Our facility is a certified NHSF (Non-Hospital Surgical Facility), approved by all three pertinent governing bodies: the CDSA, CPSA and AHS. Undergoing this rigorous accreditation process allows us to offer full general anesthesia administered by a medical anesthesiologist. This means you’ll have two doctors looking after you while you’re asleep to keep you safe and healthy. Despite this, there are always risks with any method of anesthesia, whether in the hospital or in an outpatient surgical facility such as ours, and the level of risk is mostly related to any co-morbidities you have.
How long will the procedure take?
This varies based on how difficult the teeth are, and the type of anesthesia or sedation utilized. On average, it takes 10-20 minutes to remove a set of all four wisdom teeth. Remember — the faster the procedure, the less swelling you’ll have, and the quicker you’ll heal up.
What are the risks associated with having my wisdom teeth removed?
 Having your wisdom teeth removed is an extremely safe and predictable procedure, however there are some uncommon complications to keep in mind. Dr. Robertson will be able to estimate the likelihood of each one for your particular case:
Having your wisdom teeth removed is an extremely safe and predictable procedure, however there are some uncommon complications to keep in mind. Dr. Robertson will be able to estimate the likelihood of each one for your particular case:
1) Damage to the nerve that runs through your lower jaw and gives sensation to the lower lip and chin (the inferior alveolar nerve), or damage to the nerve that gives sensation to the tongue (the lingual nerve). Generally there is about a 2-3% chance of this occurrence, and the majority of these cases totally resolve on their own with time. These nerves are only sensory – they do not affect your ability to speak or move your lips. This complication is more common in patients over the age of 25.
2) Sometimes a residual hole between the mouth and the sinus cavity can remain patent after removal of an upper wisdom tooth. Again, this is very rare (<1%), and is more common in patients over the age of 25. If it occurs during surgery, Dr. Robertson will repair it right away, and it will usually heal up. In very rare cases, an additional procedure may be required to repair the hole.
3) If the wisdom tooth is tucked right up against the molar in front of it (the 2nd molar), occasionally removal of the wisdom tooth can damage the tooth root of that 2nd molar. Again, this is extremely rare (<1%), and more common in patients over the age of 25.
What are the risks if I choose NOT to have my wisdom teeth removed?
Some people choose to keep their wisdom teeth, and that is a perfectly acceptable choice to make – as long as you know the risks. Studies have shown that a young adult who chooses to keep their completely asymptomatic wisdom teeth has a 64% risk of requiring at least one to be removed over the following 20 years. The main reason is since they are very far back and often partially covered by gum tissue, they can be very difficult to keep clean. This makes them prone to cavities and a special type of gum disease called pericoronitis. The tooth can also cause bone loss on the back part of the second molar, or even resorption of the root of the second molar or surrounding bone. Some studies suggest retained wisdom teeth can cause orthodontic crowding of the front teeth. If the tooth is impacted, it can still become carious or infected via a tract down the back side of the second molar, or it can develop a cyst around the crown (dentigerous cyst). Occasionally they can cause pain, pressure and/or headaches. The presence of a third molar also increases the likelihood of having a jaw fracture through that area in a traumatic situation.

Why are wisdom teeth more difficult to remove than other teeth?
Wisdom teeth are generally more difficult to remove because 1) they are further back in the mouth making access to the area difficult, and 2) they are often impacted, requiring an incision in the gums to access the area. Lower wisdom teeth in particular often require some bone removal around the teeth to make space for them to be removed, or the tooth may need to be surgically cut into pieces to facilitate safe removal.
How much does it cost to have my wisdom teeth removed?
Each case is different; it depends on the level of anesthesia desired and the complexity of the teeth. After your consultation (but before your surgery), you will be given an exact cost breakdown, inclusive of any insurance coverage for the procedure. To make it easy for you, we can even bill your insurance company directly so that you only pay the difference.
Will I feel pain during the procedure?
No, you will not feel any pain during the procedure. However, if you are having your procedure done with just freezing (local anesthesia) or IV sedation, you may feel some pressure and vibrations from the drill. If this is a concern for you, general anesthesia may be a better option. If you have general anesthesia for your procedure, when you wake up your whole mouth will be numb from freezing that’s placed while you’re asleep. This type of freezing lasts 4 – 8 hours, which is designed to keep you comfortable while you get home and settled.
Will I have stitches?
Dr. Robertson stitches up all lower wisdom tooth sites to ensure the best chance of uncomplicated healing, although sometimes top wisdom teeth do not require stitches. The stitches are resorbable, which means the part under the gums will dissolve and then they fall out. This typically occurs within 3-5 days, but occasionally longer lasting stitches are used.
What is a dry socket?
Normally after a tooth is removed, a blood clot forms at the site of the surgery. Over time this blood clot turns into new gum and bone. A dry socket occurs when the blood clot is lost at some point after surgery (usually 3-5 days after the procedure). The symptoms are a sudden increase in radiating or throbbing pain and a bad taste in the mouth.
How can I minimize the risk of getting a dry socket?
 The lower third molar is the most likely site in the whole mouth to be affected by a dry socket, so sometimes it is unavoidable. However, there are some things you can do to reduce the risk. If you are a smoker, do not smoke for at least a week after your surgery! Smoking significantly increases your risk of a dry socket. Again, patients over 25 are more likely to experience dry sockets. Other risk factors include female gender, pre-existing pericoronitis (gum disease) at the site and a more difficult surgery (requiring bone removal and additional surgical time). If you are at a high risk of a dry socket, Dr. Robertson may place a collagen plug in the socket to try to minimize this risk.
The lower third molar is the most likely site in the whole mouth to be affected by a dry socket, so sometimes it is unavoidable. However, there are some things you can do to reduce the risk. If you are a smoker, do not smoke for at least a week after your surgery! Smoking significantly increases your risk of a dry socket. Again, patients over 25 are more likely to experience dry sockets. Other risk factors include female gender, pre-existing pericoronitis (gum disease) at the site and a more difficult surgery (requiring bone removal and additional surgical time). If you are at a high risk of a dry socket, Dr. Robertson may place a collagen plug in the socket to try to minimize this risk.
What is the expected recovery period for removal of wisdom teeth?
Recovery time is different for everybody. Dr. Robertson can often give you an estimate before surgery based on the difficulty of the teeth, your health, and your age. However, recovery time is still somewhat unpredictable. For an average 20 year old patient undergoing removal of four impacted wisdom teeth, you should plan to be off work/school for about 2-4 days. After this time, you will generally be able to do all your normal activities (except strenuous physical activity), even if you’re still a bit sore. For patients over 25 years old, the recovery time may be a little longer.
How soon can I start exercising after having my wisdom teeth removed?
For strenuous physical activity including working out, running, or heavy lifting at work, generally it is best to allow a full 7 days off. By this time, you may engage in light physical activity that elevates your heart rate moderately. If you experience throbbing pain at your surgical sites with this increase in heart rate, you should rest a little longer. However, if you experience no pain with an increased heart rate, it is generally safe to advance to full physical activity as tolerated.
Will I swell up after my wisdom teeth are removed?
Yes, absolutely everybody experiences some amount of swelling after a surgical procedure such as removal of a tooth, however the amount of swelling is extremely variable from person to person. Swelling also depends on the complexity of tooth removal and the amount of surgical time required. The swelling generally occurs in the cheeks next to the lower wisdom teeth and it peaks at about 3 days after surgery before it gradually comes down over the following two weeks. You may also experience some minor bruising of the cheeks or just under the lower jaw.
What can I eat after my wisdom teeth are removed?
At first, you should stick to foods that are easy on your mouth and stomach, such as clear liquids, yoghurt, lukewarm soup, or meal replacement shakes. However, you may advance to soft mushy foods as soon as you are feeling up to it, and then continue to advance your diet back to normal as tolerated over the next few days. However, if you have had lower wisdom teeth removed, you may have small pockets which could collect food and debris, so you need to be careful to keep these areas very clean. The best way to do this is to avoid foods with small hard bits and pieces (such as popcorn kernels, seeds, rice, etc.), and to gently rinse your mouth with warm salt water after every time you eat.
What if I have questions prior to surgery?
At the time of your consultation, Dr. Robertson will discuss your specific situation in detail. We encourage you to ask any questions you may have at this time, but if you have any follow up questions, you can give us a call at 403-263-5193 to speak to one of our patient care coordinators. More detailed information about post-operative instructions can be found here.
What instructions do I need to know for the day of surgery?
The detailed pre-operative instructions can be found here, however if you are having IV sedation or general anesthesia, two rules in particular are extremely important
- You must not have anything to eat or drink after midnight the night before your surgery.
- You must have arrangements for a responsible adult to drive you home once you have finished your surgery.

